4 Signs of a Quality Primary Care Provider
Finding a high-quality primary care provider is essential for maintaining long-term health and overall wellness. As the first point of contact for most medical concerns, a primary care provider (PCP) plays a critical role in disease prevention, chronic condition management, and navigating the healthcare system. With so many providers available, however, it can be difficult to determine which one is truly reliable and effective. This article outlines the key qualities of a great PCP, helping individuals make informed choices about their healthcare.
1. Comprehensive Communication Skills
Active listening is a fundamental skill that distinguishes a superior primary care provider from an average one. When providers engage in active listening, they demonstrate genuine interest in the patient's concerns, taking the time to fully comprehend and reflect on the information presented. This engagement results in more accurate diagnoses and personalized treatment plans, ultimately enhancing patient satisfaction. Additionally, by recognizing non-verbal cues, a PCP can address issues that a patient may not explicitly verbalize. Active listening not only improves healthcare outcomes but also fosters a trusting relationship between the provider and patient, which is essential for continuity of care.
The utilization of open-ended questions by primary care providers serves as a cornerstone of effective patient communication. These questions invite patients to share detailed information regarding their symptoms and concerns, providing a broader context for diagnosis and treatment. Instead of yes or no responses, patients are encouraged to express themselves more freely, allowing the PCP to gain deeper insights into their health status. The ability to ask the right questions efficiently can significantly alter the trajectory of patient care, ensuring that no key information is overlooked. This comprehensive approach is vital, especially in complex cases where symptoms may overlap or persist across multiple systems.
Empathy is integral to the practice of medicine, yet it is often underestimated in clinical settings. An empathetic primary care provider can perceive and understand a patient's feelings and perspectives, creating a supportive and comforting environment. This emotional intelligence is paramount in addressing sensitive health topics, such as mental health or end-of-life care, where patients may feel vulnerable. Empathetic engagement is linked to increased patient satisfaction and trust, encouraging open and honest communication that is essential for quality care. Furthermore, empathy strengthens the provider-patient relationship, likely resulting in better patient cooperation and long-term health benefits.
2. Accessibility and Availability
Efficient appointment scheduling is another critical aspect of availability in primary care. By implementing user-friendly scheduling systems, providers make it easier for patients to book appointments at their convenience. This efficiency reduces stress and ensures that patients are seen in a timely manner, fostering trust in the healthcare system. Furthermore, accommodating last-minute appointments or emergency visits exemplifies the provider’s commitment to patient-centered care.
Flexible office hours are a strong indicator of a primary care provider’s commitment to meeting the diverse needs of patients with varying schedules. Providers who offer evening or weekend appointments make it easier for working professionals, students, and busy families to access care without disrupting their daily routines. According to the U.S. Bureau of Labor Statistics, there were about 112,010 family medicine physicians as of 2023, highlighting the importance of choosing one who prioritizes patient-centered accessibility. Extended hours not only improve convenience but also reduce unnecessary emergency room visits for non-urgent issues. This approach ultimately makes healthcare more accessible, efficient, and effective for all patients.
Comprehensive follow-ups are essential in maintaining continuity of care after consultations or procedures. By systematically conducting follow-ups, PCPs ensure that treatment plans are effective and that patients are recovering as expected. Regular follow-ups demonstrate the provider's commitment to holistic care and patient well-being. Furthermore, follow-up appointments allow patients to address any lingering questions or concerns that may have arisen since their last visit. For chronic health conditions, in particular, consistent follow-ups are crucial in monitoring progress and adjusting care plans as necessary, contributing to better health management.
3. Patient-Centered Approach
One of the hallmarks of a patient-centered approach is the development of individualized care plans. These plans are tailored to address the unique needs, preferences, and circumstances of each patient, ensuring personalized and relevant care. Individualized care plans consider factors such as medical history, lifestyle, and socio-economic status, which can impact treatment success. By crafting a care plan that resonates with the patient's life, PCPs improve adherence and outcomes. Additionally, personalized care reflects a provider's commitment to treating patients as holistic individuals rather than just addressing specific symptoms or illnesses.
Involving patients in decision-making is a cornerstone of the patient-centered care model. Empowering patients to take an active role in their health decisions reinforces their autonomy and promotes a collaborative relationship with their PCP. Providers who engage patients in discussions about treatment options, risks, and outcomes enhance their understanding and commitment to the chosen course of action. This collaborative approach fosters trust and satisfaction, leading to better health behaviors and outcomes. Involving patients in decisions also respects their preferences and values, which are critical components of personalized healthcare.
Building long-term relationships with patients is central to fostering trust and continuity of care. PCPs who prioritize establishing strong connections with their patients create an environment where individuals feel comfortable sharing personal health information. Long-term relationships enable providers to develop a detailed understanding of a patient's history, preferences, and evolving health needs. This knowledge facilitates more accurate diagnoses, personalized interventions, and preventative care measures. By investing in long-term relationships, PCPs help to ensure early detection of health issues and promote lasting health outcomes.
4. Emphasis on Preventive Care
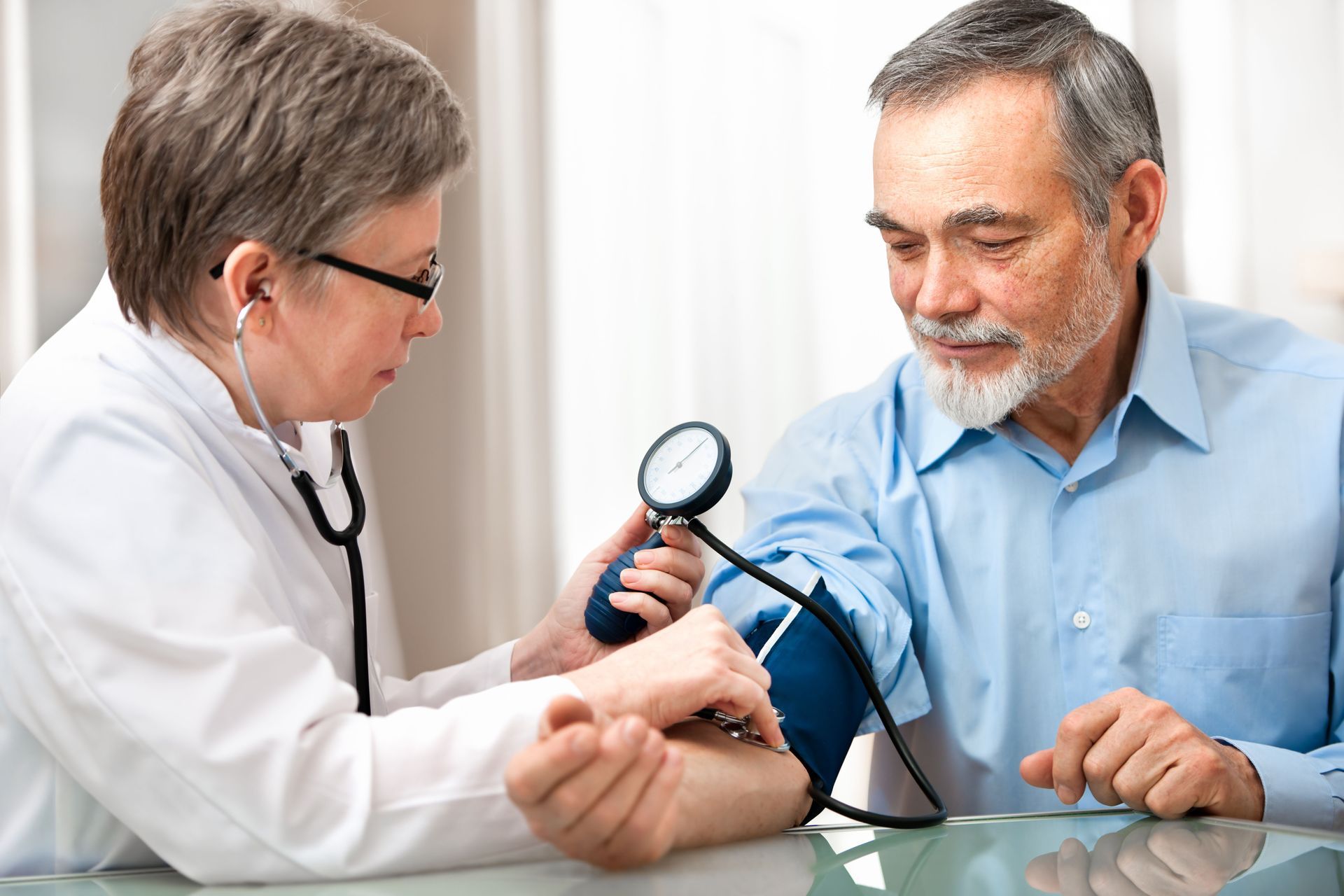
The inclusion of routine screenings is a proactive measure a quality PCP will take to prevent and detect diseases early. Regular screenings for conditions such as high blood pressure, diabetes, and cancer can significantly improve patient outcomes through early intervention. By adhering to updated screening guidelines, PCPs can effectively mitigate health risks for their patients. Routine screenings represent a preventive approach to healthcare, enabling the detection of asymptomatic conditions before they become serious. This emphasis on prevention illustrates the provider's commitment to maintaining patients' long-term health and well-being.
Proactive health monitoring is an essential aspect of preventive care, involving regular assessment of patient health metrics and risk factors. By tracking vital signs, lab results, and lifestyle choices, a primary care provider can identify and address potential health issues before they escalate. This proactive approach allows patients to better understand their health and take early action when necessary. Continuous monitoring fosters an environment of shared responsibility for health between the provider and patient. As a preventive strategy, proactive health monitoring can significantly reduce healthcare costs and improve long-term outcomes.
Risk assessment plans are personalized strategies designed to identify and manage potential health risks. These plans involve evaluating genetic, environmental, and lifestyle factors that could contribute to health issues. By developing individualized risk assessments, PCPs can implement targeted interventions to mitigate risks and prevent disease progression. Comprehensive risk assessments empower patients with the knowledge they need to make informed health choices. Such plans demonstrate a provider's commitment to preventive care and proactive disease management, ensuring better health outcomes.
Choosing the right primary care provider is an investment in long-term health, comfort, and peace of mind. By focusing on communication, accessibility, preventive care, and a patient-centered approach, individuals can confidently select a provider who truly supports their well-being. Ultimately, a trusted primary care provider becomes a reliable partner in navigating the complexities of healthcare and achieving lasting wellness. Contact Troy Medical, P.C. to speak to a qualified and compassionate primary care professional.



Share On: